Weak spot of antibiotic-resistant bacteria found
New research published in the journal Nature reveals an Achilles’ heel in the defensive barrier which surrounds drug-resistant bacterial cells, Sciencedaily.com reports.
The findings pave the way for a new wave of drugs that kill superbugs by bringing down their defensive walls rather than attacking the bacteria itself. It means that in future, bacteria may not develop drug-resistance at all.
Outer membrane
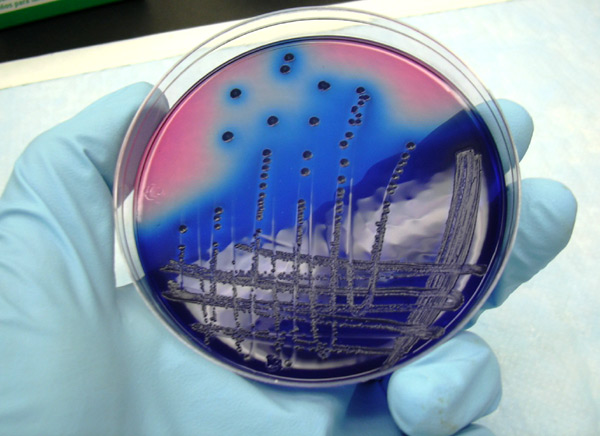
Researchers investigated a class of bacteria called ‘Gram-negative bacteria’ which is particularly resistant to antibiotics because of its cells’ impermeable lipid-based outer membrane. This outer membrane acts as a defensive barrier against attacks from the human immune system and antibiotic drugs. It allows the pathogenic bacteria to survive, but removing this barrier causes the bacteria to become more vulnerable and die. Until now little has been known about exactly how the defensive barrier is built. The new findings reveal how bacterial cells transport the barrier building blocks (called lipopolysaccharides) to the outer surface.
Current antibiotics are useless
Group leader Prof Changjiang Dong, from UEA’s Norwich Medical School, said: “We have identified the path and gate used by the bacteria to transport the barrier building blocks to the outer surface. Importantly, we have demonstrated that the bacteria would die if the gate is locked. This is really important because drug-resistant bacteria is a global health problem. Many current antibiotics are becoming useless, causing hundreds of thousands of deaths each year”.
Antibiotic use in animals
Antibiotic use in livestock is often named as the main reason for antibiotic resistance bacteria and hence the problems caused for human health. Antibiotics in general must be used judiciously in animals and humans because both uses contribute to the emergence, persistence, and spread of resistant bacteria. Livestock may serve as a reservoir of resistant pathogens and resistance mechanisms that can directly or indirectly result in antibiotic resistant infections in humans, but also the use of antibiotics in humans are causing the worldwide increase of resistant bacteria.
This research was funded by Wellcome Trust. Research collaborators included the University of St Andrews, Dr Neil Paterson of Diamond Light Source (UK), Dr Phillip Stansfield from the University of Oxford, and Prof Wenjan Wang of Sun Yat-sen University (China).
Source: Sciencedaily.com











